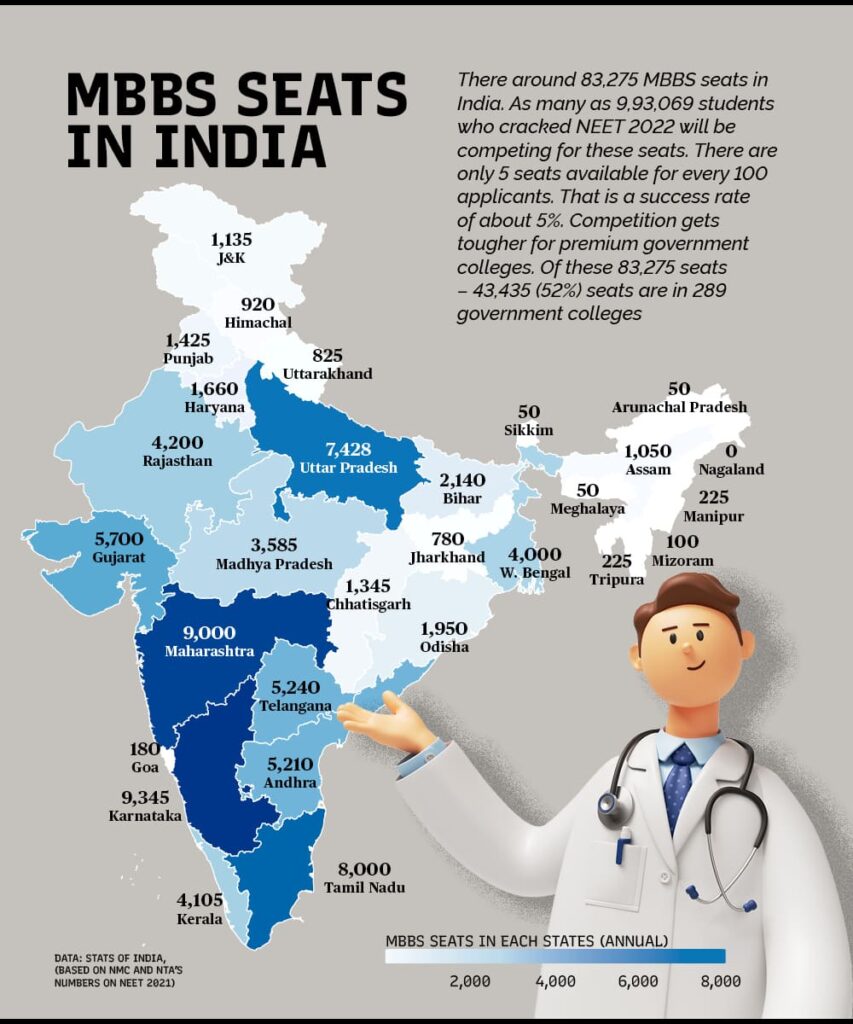
India’s Medical College Seats Insufficient- Probable Solution. Total No: of Aspirants- 9,93,000: Total No: of Seats- 83,000 Spots
Every year, about 7 lakh students fight for nearly 80,000 medical college seats in India. Due to high enrolment numbers, a whopping 9,93,069 students have managed to clear NEET 2022 and will be contending for the same number of seats. To make matters worse, several study-abroad options including China, Ukraine, and the Philippines are yet to invite Indian medical aspirants back on campuses due to geopolitical reasons, including the Covid-19 pandemic. This makes several study-abroad aspirants look for options in India.
While the easy way out seems to be to set up more medical colleges, doing so has several policy hurdles. To establish a medical college, the minimum requirements include 20 acres of land and that the management should have been operating a hospital for the previous two years, as per existing rules. Limited land availability and high land prices have pushed newer medical colleges in tier-3 cities or rural areas. However, medical colleges along with a hospital in rural areas are unable to attract faculty and doctors.
With an almost stagnant number of seats but an increasing number of medical aspirants, many experts have demanded to recognise hybrid learning in the medical sector as a solution to the seat crunch. Since a majority part of the MBBS, BDS and allied courses are theoretical, experts say that having online or hybrid sessions for the theory part and making students attend classes for practical and emphasis on clinical practice can solve the problem. Currently, the government does not accept online as a mode for medical studies.
Accepting online education for certain parts of the medical course can not only solve the immediate crisis at hand which includes Indian medical students studying in Ukraine-, China-, and Philippines-based universities who are stuck in India but will also ensure students who have scored lower in NEET also get a seat, believes Nalin Saluja, Co-Founder, and CTO at Virohan — an educational institution in Faridabad, Haryana which offers paramedical courses.
“Online education is great in terms of providing a level playing field to learners. New doctors prefer to stay in tier 1 & tier 2 cities as most of their seniors practice there. The opportunity to learn from them and improve their own practice is very high if they practice directly under their seniors or with any celebrity doctor. If online education is blended with effective hands-on training or mentorship, then every clinician from across the country can build similar capabilities and competencies. Similarly, they can influence other medical professionals in their regions to invest in upskilling and grow their own practice/career,” Dr. Amrit Das, co-founder of Medstudies.
LIMITED QUALITY FACULTY
The problem ultimately boils down to the low doctor-patient ratio. India has one doctor for 2,000 patients for primary care and an extremely low doctor-patient ratio for specialists for one doctor for more than 5,00,000 patients. Some of these doctors are further responsible for training medical students.
“The shortage of skilled medical professionals is a major reason for the inadequate healthcare system in India. This is more so in rural India. Lack of proper infrastructure, amenities, and proper remuneration is the reason why doctors shun rural postings. Proper upgradation of district and taluk level hospitals as well as PHCs will lead to an improvement and attract qualified health professionals to rural areas. Public Private partnership working in sync will go a long way in mending this gap,” said Vindya Subbiah, senior vice president, Academics & Research, Milann Fertility Centre.
“The value a student gets in a classroom setting cannot be replaced, but even in qualified and top-ranking colleges, faculty is in shortage. With high demand, top faculties are limited to high-ranking colleges and tier 2 and tier 3 colleges end up having to fight for quality faculty members. This issue can be sorted if one high in-demand medical professional can share lectures with a wide range of students using technological platforms,” said Nalin Saluja, co-founder and CTO at Virohan, who trains paramedical staff using a similar model.
NEED FOR FRAMEWORK
Experts recognise that there is a lot of apprehension around the use of edtech platforms for training future doctors considering the high stakes involved in the jobs. There is a need for a narrow assessment and critical review process before adopting online modes. India currently lacks any such policy.
Solving this problem requires all stakeholders to work toward creating a quality framework. The digital transformation will not be faultless, but a process of trial and error where growth would be much more organic through continuous learning and feedback. The solution would be to integrate digital innovations concurrently without tedious analysis and deep evaluation to study the benefit of applying hybrid modes of learning, said Dr. Das.
“Various studies have identified time constraints, propensity to get distracted, poor technical skills & training, and inadequate behavioural training of both the student and educator as some of the reasons for ineffective online instruction. All these challenges can be solved through proper training, setting up of right expectations, and improvising content mediums and delivery. Of course, hands-on clinical skills training would still be imparted best through physical interactions,” suggested Dr. Das , adding that the question is not if online education will be able to support high stakes but to identifying the potential challenges with online/ hybrid modes and working to fill those gaps.
The students are very much interested in innovative teaching methods but a frequent argument behind the slow adoption of online learning was that its implementation was time-intensive, expensive, and lacked the required infrastructure.
The present conditions offer a unique opportunity for the modernisation of medical learning to cater to the students’ needs and many opinions are shaping up on the delivery of medical education in the future. This can be started by training paramedics, and patient care staff and recognising training of existing medical professionals via online modes, suggested Dr. Das.
By: Amrit Das